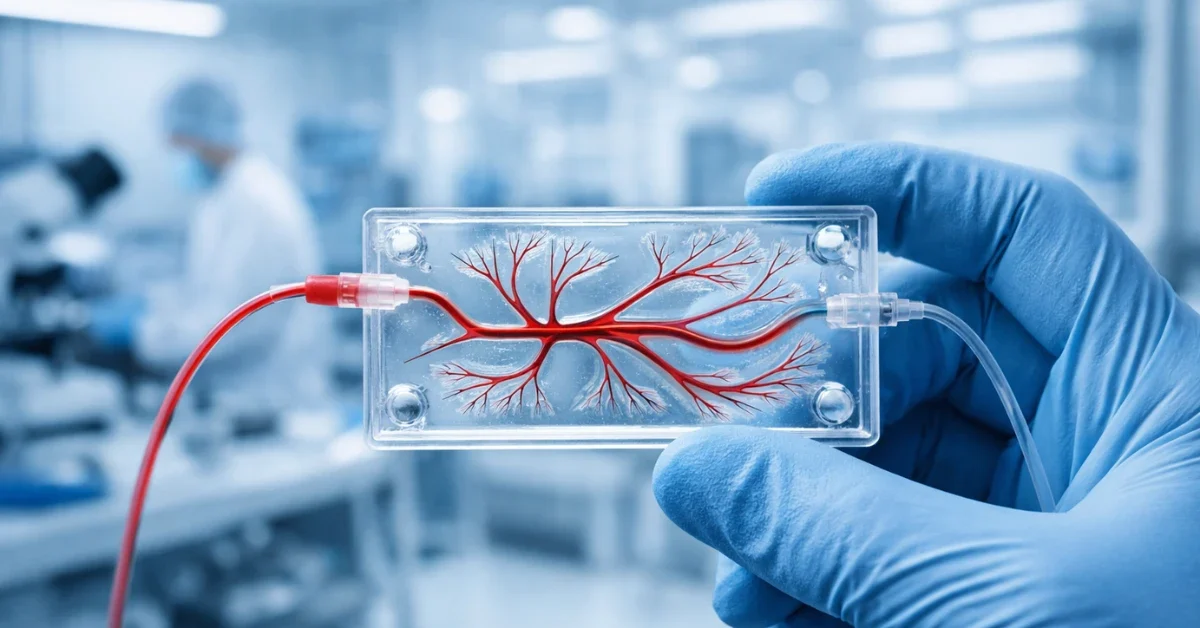
Scientists have reached a significant milestone in medical research by developing highly realistic engineered blood vessels that could change how we treat heart and vascular conditions. This breakthrough uses “vessel-on-a-chip” technology to create living models of human arteries and veins. These tiny, transparent devices allow researchers to see exactly how human cells react to blood flow and medicine in real-time, offering a level of detail that was previously impossible.
Vascular diseases, including atherosclerosis and blood clots, remain a leading cause of death worldwide. For decades, medical researchers have relied on animal testing to find new treatments, but these results often do not translate to human patients. The development of these advanced engineered blood vessels provides a more accurate way to study human biology and speed up the discovery of life-saving drugs.
The problem with traditional medical research
For years, the pharmaceutical industry has faced a high failure rate when moving potential drugs from animal trials to human clinical tests. One major reason for this is that the vascular systems of mice or rats do not function exactly like those of humans. Animal models often fail to show how a human blood vessel will respond to the complex pressures and chemical signals found in our bodies.
Researchers at Texas A&M University, led by Dr. Abhishek Jain, have focused on solving this problem by building human systems outside of the body. By using human cells on microchips, scientists can create a controlled environment that mimics the human circulatory system. This approach reduces the need for animal testing while providing data that is much more relevant to human health.
Replicating the complexity of human anatomy
One of the most innovative aspects of this new technology is its ability to replicate the complex shapes found in the human body. Natural blood vessels are not just straight tubes; they are full of curves, twists, and branches. These geometric features are critical because vascular diseases like atherosclerosis—the buildup of plaque—usually begin at these specific points of curvature and branching.
The new engineered blood vessels are designed to include these realistic geometries. By using advanced manufacturing techniques like microfluidics and 3D bioprinting, scientists can create chips that feature the exact curves and bifurcations found in human arteries. This allows them to study how blood flow patterns change at these junctions and why certain areas are more prone to developing disease than others.
Understanding the power of shear stress
Blood flow does more than just transport oxygen; it also applies a physical force known as shear stress to the walls of the blood vessels. This mechanical force is a key player in vascular health. Endothelial cells, which line the inside of our blood vessels, are extremely sensitive to this stress. When blood flows smoothly, these cells stay healthy, but when the flow becomes turbulent near a curve or a blockage, the cells can become inflamed.
By using engineered blood vessels, researchers can precisely control and measure these biomechanical forces. The chips allow for “pulsatile flow,” which mimics the rhythmic beating of the human heart. This gives scientists a front-row seat to see how endothelial cells and smooth muscle cells interact under the same stresses they would face inside a living person. Observing these interactions helps identify the exact moment a vessel begins to fail or develop a clot.
Improving drug testing and safety
The ability to test new medicines on realistic human tissue before they ever reach a patient is a game-changer for drug safety. Pharmaceutical companies can use these engineered blood vessels to screen thousands of chemical compounds to see which ones effectively treat inflammation or prevent clotting. Because the chips use human cells, the results are much more predictive of how a patient will actually respond.
This technology also allows for personalized medicine. In the future, doctors could potentially use a patient’s own cells to create a custom “vessel-on-a-chip.” This would allow medical teams to test different dosages or combinations of medications on a model of that specific patient’s vascular system to see which treatment works best before the patient even takes a pill.
A new era for vascular health
The move toward organ-on-a-chip technology marks a shift in how the medical community views disease. Rather than looking at a whole organism, scientists can now zoom in on the specific cellular and mechanical triggers of illness. These engineered blood vessels represent a bridge between laboratory research and clinical application, providing a faster and safer path to new therapies.
As this technology continues to evolve, it is expected to play a major role in studying other conditions, such as the way cancer cells travel through the bloodstream or how the blood-brain barrier protects the central nervous system. For now, the focus remains on the heart and vessels, where these tiny chips are making a massive impact on the future of human health.